$200 Billion Reality Check: What Healthcare Achieved, What It Missed, and What AI Could Have Saved


2025 began with conviction. New CMS mandates, record labor shortages, and unrelenting administrative costs created the perfect environment for AI to deliver real financial relief.
In our State of AI During the Great Burnout survey published in late 2024,
- 82% of healthcare leaders said AI was essential to operations
- 71% planned to start with documentation automation
- 85% of CIOs warned that fragmented point solutions would create more problems than they solved
The goal was clear: reduce administrative waste, improve margins, and give time back to care teams. Twelve months later, optimism remains, but the results tell a different story.
How 2025 Is Ending: Costs Remain High, Complexity Higher
Menlo Ventures projects that the U.S. healthcare system will spend roughly $740 billion on administrative functions in 2025. That figure represents the total administrative burden across providers and payers, much of it still tied to manual processes that add cost without improving care.
The paradox is that adoption has never been higher. Menlo’s research shows healthcare organizations adopting AI at more than twice the rate of the broader economy. Within two years, the sector moved from early curiosity to widespread experimentation, with 1 in 4 health systems now deploying AI in documentation, coding, or revenue operations.
For CFOs and COOs, this wave of adoption brought both momentum and frustration. Investment reached $1.4 billion, most of it directed toward administrative automation. Yet the results remain uneven.
Three structural barriers have slowed progress.
First, adoption has been siloed, with AI tools for eligibility, documentation, and claims operating independently.
Second, data fragmentation across vendors continues to create integration bottlenecks.
Third, pilot fatigue has taken hold as teams test multiple solutions without advancing to full deployment.
In Flow’s 2024 survey, 85% of CIOs predicted that fragmented approaches would generate new inefficiencies instead of solving existing ones. By the end of 2025, their prediction has largely come true.
AI has delivered value, but not yet unity. The technology is here. What’s missing is connection.
Where Healthcare Fell Short: The Price of Fragmentation
By late 2025, the industry’s progress had a clear pattern: more AI, but not more alignment.
McKinsey’s Generative AI in Healthcare: Current Trends and Future Outlook found that 85% of U.S. healthcare organizations have begun adopting or piloting generative AI. Yet only a small share advanced beyond limited experiments. Most confined their efforts to single-use cases rather than connected systems.

About 61% of health systems partnered with third-party vendors to build customized tools, while 19% bought off-the-shelf solutions. These decisions accelerated experimentation but hindered integration. Each deployment meant another platform, another dataset, another workflow to maintain.
McKinsey’s research found that 64% of organizations implementing AI reported measurable ROI, primarily in administrative efficiency and clinical productivity. Yet those gains stayed within departments and rarely scaled across the enterprise.
For most, 2025 ended as it began: fragmented tools, familiar inefficiencies, and unrealized savings.
What Unified AI Actually Delivered in 2025
A small number of health systems broke through the inertia of pilots and silos. They proved that when automation operates as one system rather than many, transformation follows.
These organizations unified AI across access, care, and collections, connecting front-end scheduling and eligibility with documentation, coding, and payment workflows.
The difference was not in the technology itself, but in how it was deployed. Each layer reinforced the others, creating measurable financial and operational gains within weeks.
For health systems that moved from pilots to platforms, the results were tangible.
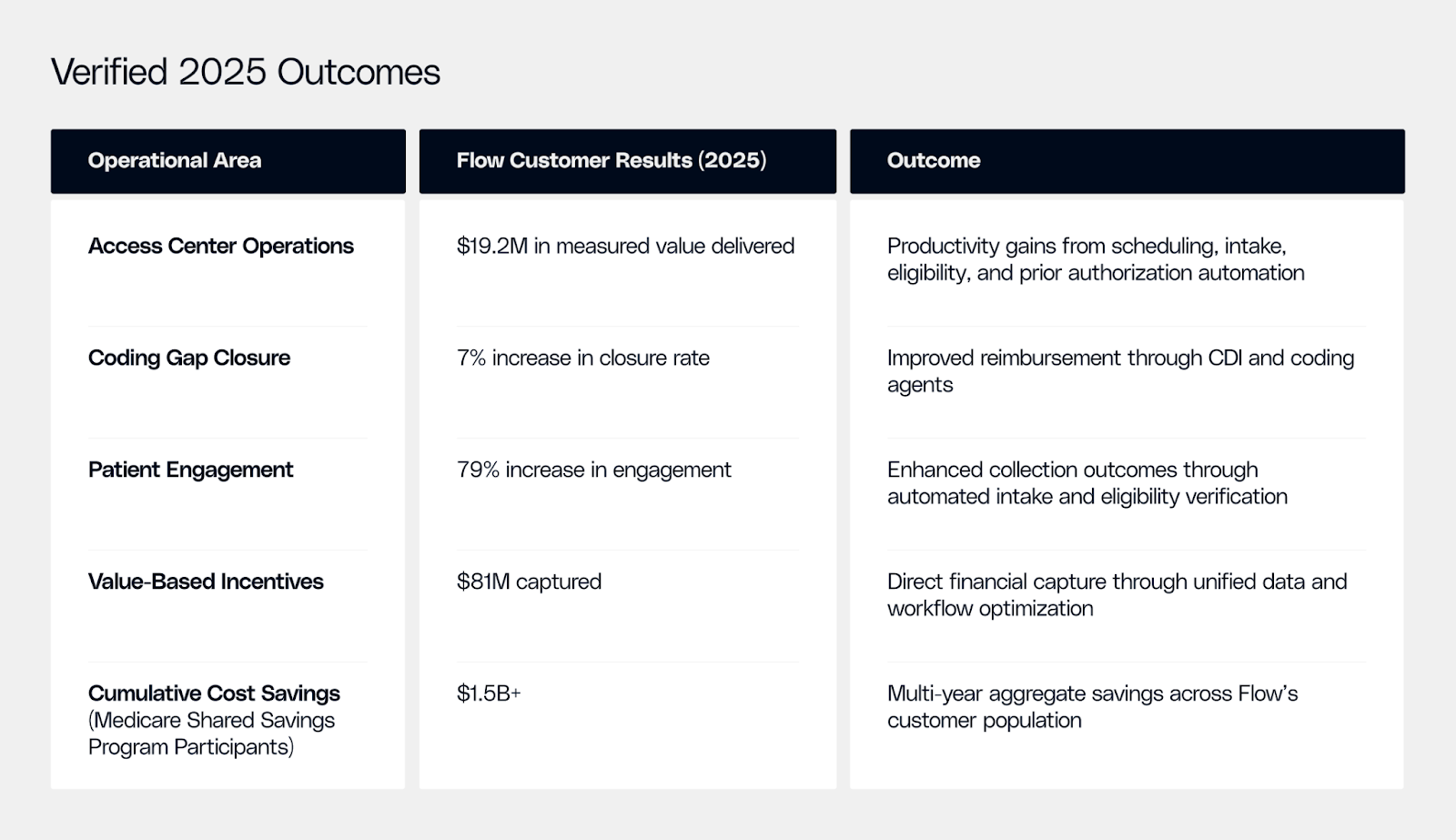
Note: These outcomes represent verified Flow customer results achieved in 2025 through documented program data and case studies. Results may vary based on implementation scope, operational maturity, and healthcare setting.
The performance pattern was consistent.
- Front-end automation increased utilization and reduced leakage.
- Mid-cycle automation strengthened documentation and cut denials.
- Back-end automation accelerated cash flow and reduced write-offs.
Each function amplified the next. A cleaner claim meant faster payment. Faster eligibility verification meant fewer denials to manage. Unified visibility turned isolated wins into systemwide performance.
Had the broader healthcare industry pursued this integrated approach at scale in 2025, it could have reclaimed between $100 billion and $265 billion in annual administrative relief, depending on implementation breadth.
The takeaway is simple but decisive. AI delivers when it is unified. Fragmentation costs money; integration compounds value.
Flow’s Role: Turning Potential into Performance
Flow was built to solve exactly this problem. It is an AI-powered financial performance platform that connects every stage of the revenue cycle into one intelligent system.
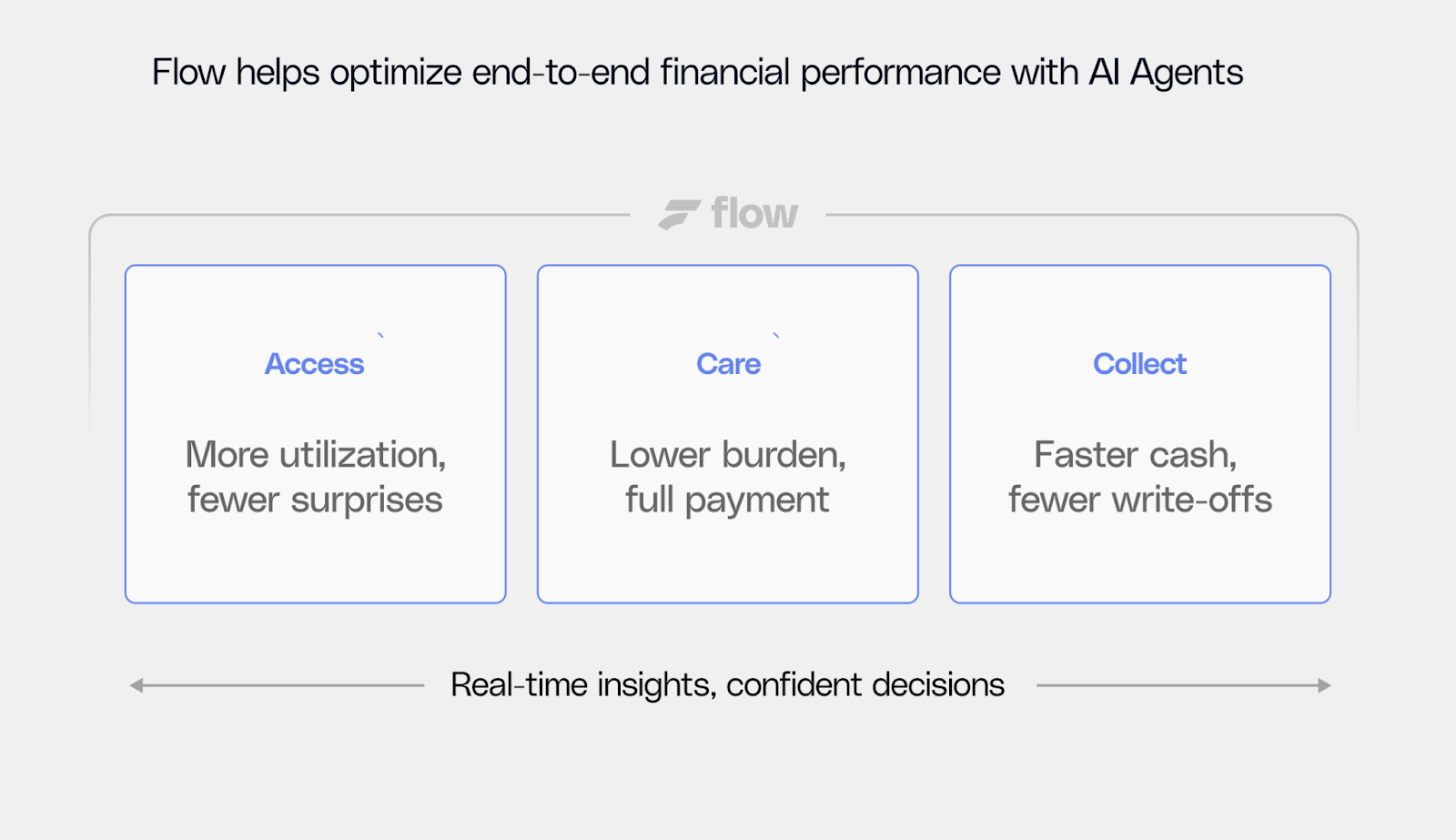
Flow Access improves revenue capture at the front end by automating scheduling, intake, eligibility verification, and prior authorization. The result: higher utilization, cleaner claims, and fewer lost encounters.
Flow Care strengthens the mid-cycle by handling documentation, coding, and CDI support. Providers spend less time on clerical work, while finance teams see more accurate, compliant reimbursement.
Flow Collect brings discipline to the back end, managing denials, appeals, and payment reconciliation to accelerate cash flow and reduce write-offs.
Together, these modules operate as a connected revenue cycle performance platform that unifies data, processes, and performance metrics across departments. CFOs and COOs using Flow report measurable gains in margin reliability, labor efficiency, and revenue predictability.
What began as point automation becomes a true financial infrastructure - a system designed not only to cut administrative waste but to optimize how revenue flows through the enterprise.
The 2026 Imperative: From Pilots to Performance
2025 was the test case. 2026 will be the inflection point. The question is no longer whether AI works, but whether leaders can make it work together.
The systems that consolidate automation across the revenue cycle will recover the savings 2025 left behind. They will measure value in millions each quarter. Not in pilot milestones.
Healthcare’s future belongs to those who unify intelligence across every workflow. Flow is helping systems lead that transition — transforming integration into lasting financial resilience.
Healthcare’s future depends on unified intelligence across every workflow. Flow is helping systems lead that transition, turning integration into sustainable margin growth, one connected operation at a time.


.png)



.png)



.avif)









.svg)
.svg)

.svg)

