Fixing the Financial Journey in Healthcare: One Intelligent Workflow at a Time

How AI-led automation can align provider revenue goals with patient trust and satisfaction
The financial side of healthcare was supposed to become more transparent, more predictable, and less painful. Instead, for most patients, it has become a maze. Even those with robust coverage find themselves facing surprise bills, cryptic EOBs, and long waits just to learn what is covered. This is not just an administrative inconvenience. It is a trust crisis that delays care, damages loyalty, and leaves millions in revenue uncollected.
On the provider side, the picture is just as stark. Front desks are flooded with coverage questions, billing teams spend hours on rework, and clinicians burn out as they wrestle with prior authorizations and paperwork late into the night. This is the crucible where patient satisfaction, financial performance, and staff well-being collide.
The Financial Experience is a Clinical Touchpoint
A patient’s last interaction with a health system is at the billing desk or in their inbox when the bill arrives. When that experience is confusing or fragmented, it can undo all the goodwill created during the clinical encounter.
Leading CFOs are starting to view the financial journey as a core part of the care experience. They are laying a foundation of proactive communication and clarity, telling patients what is covered before they arrive, providing real-time estimates of out-of-pocket costs, and sending a single, clean bill after the visit. This is a revenue protection strategy that reduces write-offs, increases throughput, and improves patient loyalty.
When patients leave confused about their bill, they remember that, not the care you delivered.
Meet Flow: A New Way to Align Revenue and Care
Most RCM tools digitize the status quo. Flow rethinks it. It is an AI-powered financial performance platform that grows revenue by removing friction from every step of the financial journey.
Built on unified healthcare data and self-learning AI agents, Flow turns siloed touchpoints into an intelligent system. Its three pillars — Flow Access, Flow Care, and Flow Collect — are designed to enhance utilization, capture more revenue on the first pass, and provide a smoother experience for patients.
Flow Access for Front Office Automation
Flow Access addresses the pre-visit bottlenecks that contribute to denied claims, no-shows, and delayed cash.
- The Scheduling Agent intelligently fills vacant time slots by aligning patient demand with provider capacity, driving highest utilization without overbooking.
- The Intake Agent captures complete demographic, clinical, and consent data digitally, lightening front desk burden while shrinking wait times.
- The Eligibility Agent checks coverage prior to check-in, saving revenue by identifying coverage issues early on.
- The Prior Authorization Agent initiates, submits, and monitors authorizations electronically, obtaining approvals within hours.
These four agents work together. As soon as an appointment is scheduled, it triggers an eligibility verification. When intake collects information, it feeds directly to authorization requirements. This leads to fuller schedules, fewer denials, less manual work, and predictable revenue.
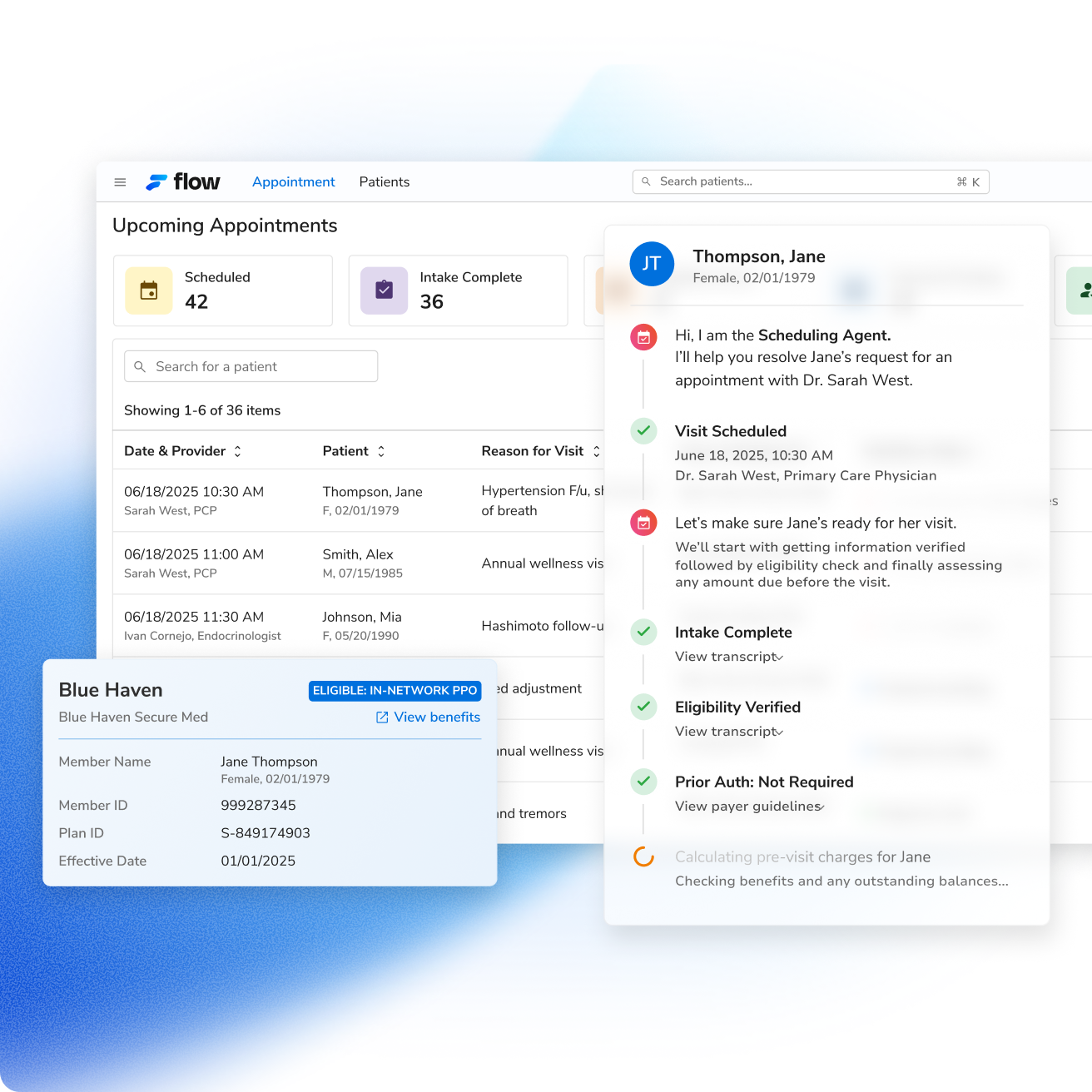
Patients notice the difference immediately. They book appointments seamlessly. Check-in takes minutes because their information is already in the system. They know what their insurance covers and what they'll owe before receiving care. Prior authorizations happen in the background so treatment doesn't get delayed.
The typical practice management friction points disappear. Patients experience a coordinated process that respects their time and reduces their anxiety about costs.
Flow Care for Removing Administrative Burden
Flow Care follows the natural progression of care delivery, eliminating documentation tasks at each step.
Before the provider enters the room, preparation happens automatically.
The Pre-visit Prep Agent collects and presents summaries of patients, illuminating care gaps and appropriate medical context.
The Care Guidelines Agent produces evidence-based recommendations tailored to the patient's medical history and case. This preparation halves pre-visit prep time. Providers enter appointments knowing what needs attention, what's overdue, and which protocols apply.
During the encounter, the Scribing Agent captures the conversation and generates notes in real-time. It creates complete SOAP notes while the visit unfolds, not hours later from memory.
Providers spend less time on documentation. They maintain eye contact and listen to the human in front of them. The computer becomes a tool, not a barrier.
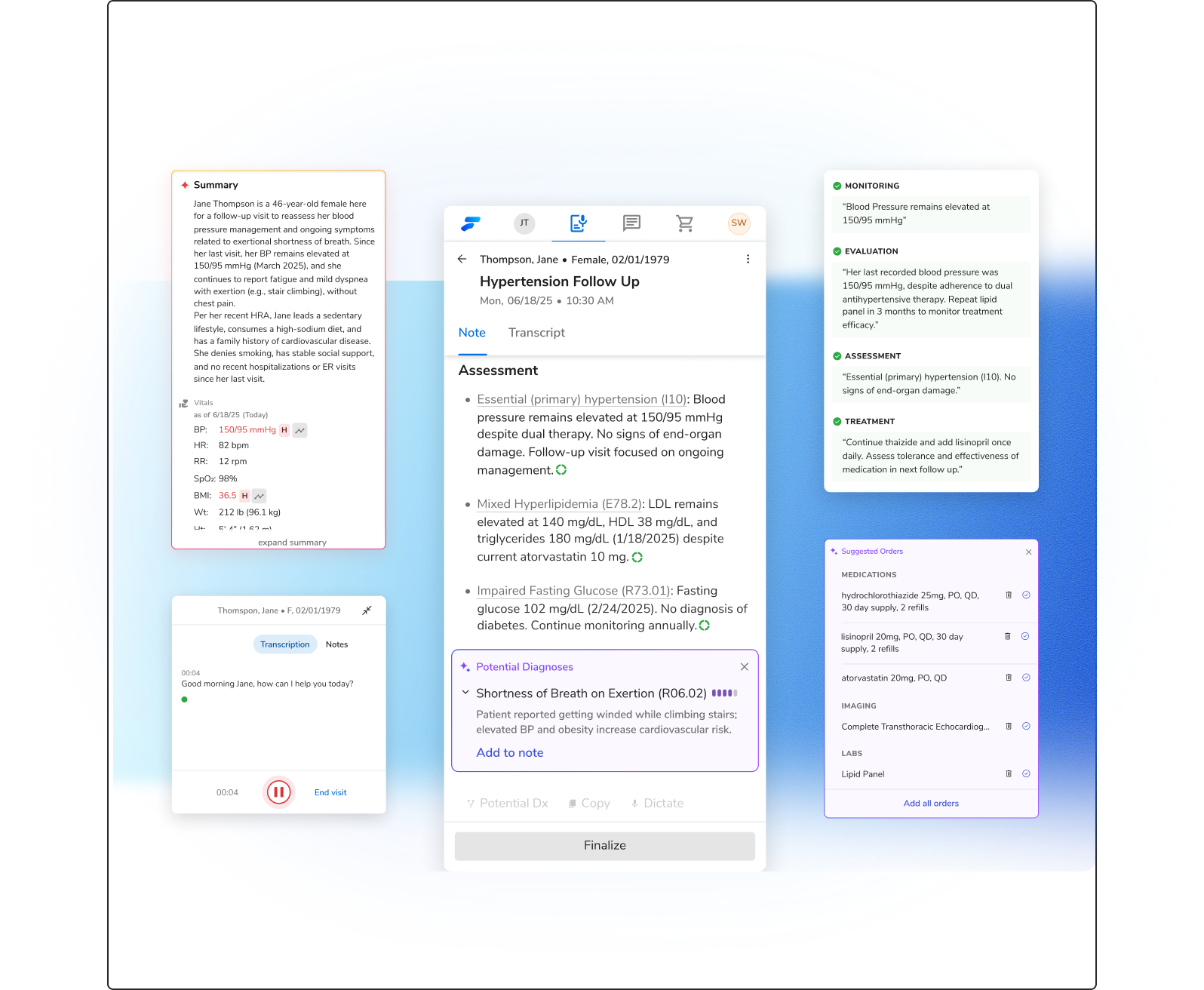
After the patient leaves, Flow ensures nothing falls through the cracks. The CDI (Clinical Documentation Improvement) Agent reviews documentation for completeness and coding accuracy. It identifies gaps that would reduce reimbursement or trigger denials, all without creating additional clinical burden.
Patients feel the difference at every stage. Their provider arrives prepared and informed. During the visit, they receive undivided attention. Follow-up happens promptly because documentation is complete before patients leave.
Flow Collect for Optimised Billing
Flow Collect converts billing from a daily firefight into a controlled, automated process that CFOs can monitor in real time. It is designed to protect margins, accelerate cash, and free staff from manual, low-value work.
Claims Submission Agent automatically builds, validates, and submits clean claims. By detecting errors upfront, it enhances first-pass acceptance and captures patient payments at the point of service; lowering downstream collections risk.
Payment Posting Agent consumes ERAs (Electronic Remittance Advice) and posts payments in a matter of hours. Reconciliation is automated, providing finance teams with near real-time visibility into cash flow and allowing staff to spend time on tricky cases rather than on manual posting.
Denial Management Agent classifies denials immediately, offers root-cause analysis, and sends them to the designated SPOC for quick resolution. This early action boosts appeal success rates and keeps claims from aging into write-offs.
Together, these agents create a continuous workflow where clean claims result in quicker payments, posting occurs automatically, and denials are addressed prior to loss of revenue. This results in predictable cash flow, decreased administrative overhead, and fewer month-end surprises.
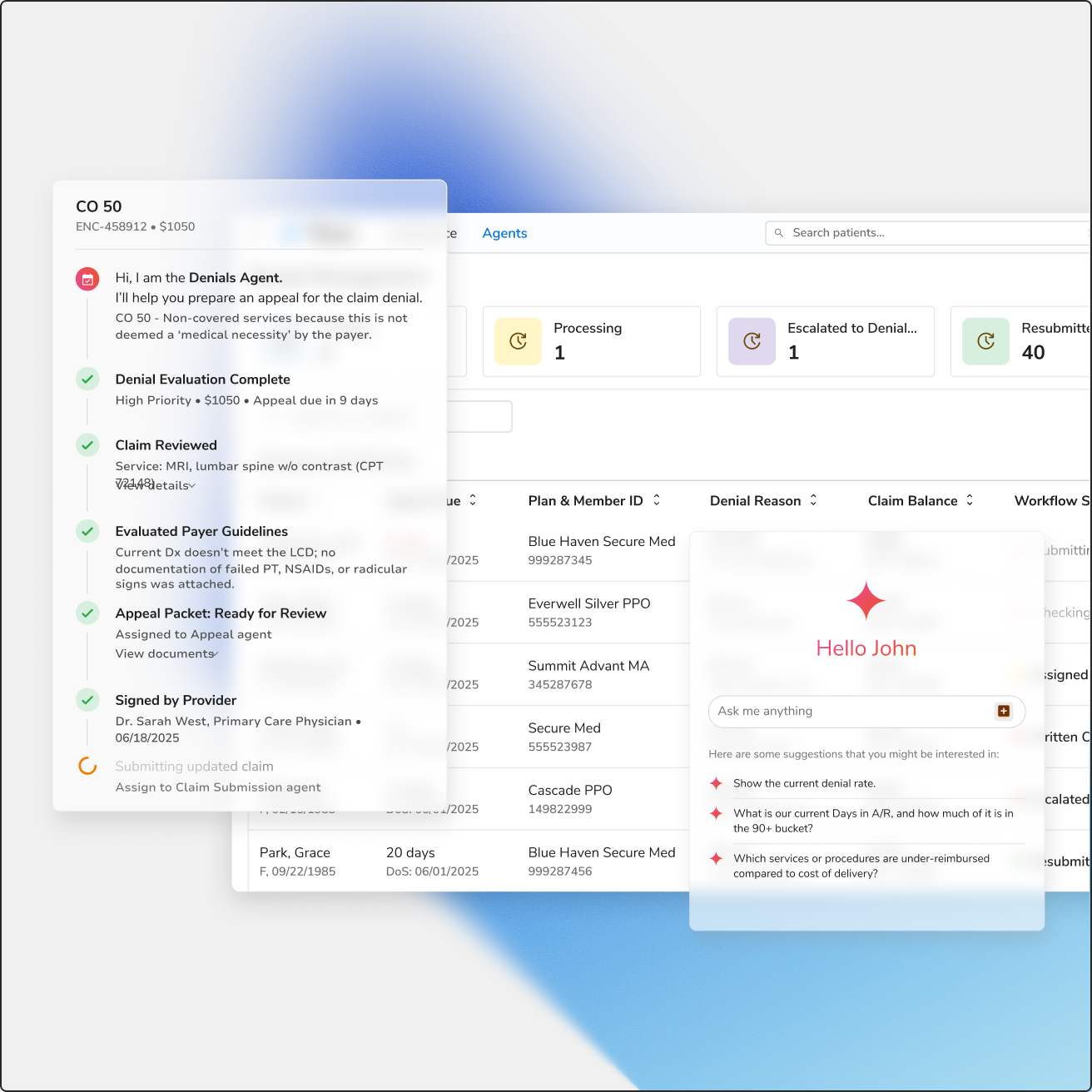
For patients, this operational accuracy means clarity. They get one accurate statement that aligns with their pre-visit estimate, with clean line items and simple payment terms. Questions get answered on the first call because staff have immediate access to the correct information. This transparency builds trust and improves loyalty.
A Day in the Life of a Digitally Empowered Clinic
It is 8:00 AM at a multi-specialty clinic. A patient books an appointment slot online the night before. The Scheduling Agent confirms availability and instantly triggers eligibility verification. By morning, the Eligibility Agent has confirmed coverage and the Prior Authorization Agent has secured approval for the procedure that will be performed.
When the patient arrives, check-in takes minutes because Intake Agent has already captured demographic and consent information. The front desk team is not chasing paperwork or making phone calls to verify coverage. Instead, they greet the patient, confirm the pre-estimate, and keep the day running on schedule.
Inside the exam room, the Pre-visit Prep Agent has collated a complete patient summary. The provider can view care gaps and pertinent history in one glance. Scribing Agent captures the encounter in real-time during the visit, allowing the provider to focus on the patient. Before the patient departs, CDI Agent ensures documentation aligns with coding requirements, eliminating the potential for downstream denials.
Following the visit, the Claims Submission Agent submits a clean claim. Payment Posting Agent applies remittances automatically as they come in. In case of a denial, Denial Management Agent flags it immediately and transfers it to the appropriate team member along with instructions for resolution.
For staff, the day feels manageable. No backlog of eligibility determinations, no stack of claims needing to be reworked, no midnight charting.
For the patient, the experience is frictionless: they see what they have to pay up front, receive timely treatment, and receive one simple statement afterwards.
This is the Flow experience. Intelligent AI made for better financial and patient outcomes.
Outcome Focus: Better Cash Flow. Happier Patients. Lower Burnout.
Revenue cycle management automation powered by AI brings measurable gains in financial performance, patient satisfaction, and employee well-being.
- Fresno Community Healthcare Network reduced prior authorization denials by 22% [1]
- University of Pittsburgh Medical Center observed a $42 million annual increase [2]
- 5-8% improvement in proper reimbursement through improved documentation [2]
- 20-25% decline in coding-related denials [2]
- Average payment realization down from 90 days to 40 days [3]
- Cost-to-collect decreases by 0.25%, that's $11.5 million saved for a $5B health system [4]
- 40% reduction in patient billing complaints with AI-driven transparency [5]
These improvements create a virtuous cycle. Better financial performance provides resources to invest in staff and patient experience. Reduced burden allows healthcare workers to focus on care. Improved satisfaction drives loyalty and referrals that strengthen market position.
Turn your Revenue Cycle from Financial Friction to Flow
The patient experience does not end when the visit is over. It ends when the bill is paid and questions are resolved. Organizations that treat financial workflows as part of the care journey protect revenue, build loyalty, and reduce staff stress.
Flow provides the tools to make this shift possible. By connecting scheduling, clinical documentation, and billing into one coordinated system, it creates a financial experience that is clear, predictable, and trusted.
The best patient experience is not just clinical. It is financial too. Now is the time to redesign it, one intelligent workflow at a time.


.png)



.png)



.avif)









.svg)
.svg)

.svg)

