Prior Authorization Beyond ePA: How AI Automates Portals, Faxes, and Calls


TL;DR
ePA works, when it works.
But it only covers a fraction of your payer mix. Most prior authorizations still move through portals, faxes, IVR, and calls—where manual work, delays, and avoidable costs add up.
The fix: AI-powered multichannel prior authorization automation that routes each request through the right path, assembles evidence once, tracks every step, and closes the loop in your EHR.
Our fix, Flow Auth, does exactly that—an intelligent prior authorization platform built for the real payer mix, automating submissions across APIs, portals, and legacy channels.
Three years ago, the ePA mandates looked like deliverance. Your revenue cycle leadership projected headcount reductions. Your CFO penciled in margin improvements.
The promise was straightforward: replace the fax machines and phone queues with clean API handshakes between your EHR and every major payer.
Reality delivered something else entirely.
The 2023 CAQH Index tells the story your operations team already knows by heart. Roughly 20% of prior authorization transactions flow through fully electronic channels.
The rest? They're trapped in the same fragmented mess that's plagued healthcare for decades. Payer portals with different login credentials for each plan. And even when your team connects through an API, one missing attachment kicks the whole request back to square one.
If you're managing 30+ locations, this is a structural drag on cash flow, patient access, and competitive positioning.
The Payer Mix Nobody Talks About in Vendor Demos
Walk into any healthcare IT pitch and they'll show you the electronic pathway. X12 278 transactions moving seamlessly from your PM system to the payer's adjudication engine. Approvals arriving in minutes instead of days. It's a beautiful vision.
Your staff lives in a different world:
| Channel | Reality in 2025 | Key Challenges |
|---|---|---|
| X12 278 / ePA | Limited payer support; even “connected” payers reject requests for missing attachments. | Incomplete data, non-standard forms, attachment-handling failures. |
| Payer Portals & IVR | Still your highest-volume channel by far. | New AI pre-screening tools increase upfront rejections, forcing rework. |
| Fax, Phone & Email | Your fallback for attachments and peer-to-peer reviews. | Format mismatches, digital-signature requirements, lost documentation. |
| Patient-Initiated Requests | Growing fast through member portals and patient apps. | Zero integration with your workflow, forcing manual data entry and rework. |

Sources: AHIMA, CAQH Index Report, Akasa, MGMA, AMA
Every portal login translates into labor hours. Every fax elongates revenue recognition. Every phone call competes with patient care.
Where ePA Breaks Down and Manual Work Reappears
Even when a payer supports ePA, four persistent failure modes drive staff back to legacy channels:

1. AI-Driven Pre-screen Rejections
- Payers use machine learning to reject incomplete submissions earlier.
- The cycle accelerates, but rework still occurs because evidence gaps persist.
2. Attachments Fail to Transfer Automatically
- EHR export gaps require manual downloads, conversions, and uploads.
- Industry time-and-motion studies estimate 14–20 minutes per attachment set.
3. Proprietary Form Fields Override Standards
- Staff toggle across systems to fill non-standard questions.
- Each context switch introduces transcription and compliance risk.
4. Complex Cases Escalate to Provider-to-payer Calls
- Peer-to-peer reviews often add multiple days to scheduling workflows.
- Post-call documentation issues can return cases to pending status.
These breakdowns cascade into postponed procedures, deferred revenue, and staff fatigue.
Downstream Financial Impact: Workforce and Patient Leakage
The 2024 AMA prior authorization physician survey show:
- 39 prior authorizations per physician per week
- 13 hours spent weekly on PA tasks
- 89 percent of physicians report PA contributes to burnout
Radiation oncology data indicates 68 percent of PAs introduce ≥5-day delays, with 78 percent of patients sometimes abandoning treatment.
Abandonment becomes direct revenue loss.
Burnout elevates recruitment and premium labor costs.
Administrative churn preserves hiring and training as chronic expense lines.
These pressures are not abstract. They reduce operating margin.
The Operating Model Shift: AI-Powered Multichannel Automation
The next generation of prior authorization automation doesn't try to replace electronic prior authorization (ePA) solutions. It treats ePA as one channel in a broader orchestration layer. Leading health systems are adopting AI-driven, multichannel operating models built on these principles:

The goal isn't to eliminate human judgment. It's to deploy your skilled staff on exceptions and escalations instead of repetitive data entry.
A Pragmatic Playbook That Flow Auth Operationalizes
Rolling out multichannel automation does not require replacing your existing systems. It requires applying intelligence to the infrastructure already in place so that prior authorization automation produces measurable financial returns within quarters rather than years.
The operating model consists of five sequential capabilities, each of which Flow Auth delivers natively:
| Operational Priority | What Flow Auth Does | Financial and Operational Outcome |
|---|---|---|
| 1. Map Your Prior Authorization Ecosystem | Real-time payer intelligence that continuously surfaces each payer’s active rules, coverage policies, and approval patterns across locations and service lines. | Establishes a definitive baseline for cycle time, approval rate, and denial drivers, creating the foundation for a credible ROI model. |
| 2. Automate Evidence Preparation | NLP extracts required clinical evidence directly from EHR documentation and structures it to match payer-specific requirements. | Reduces manual preparation time and mitigates delays from incomplete submissions. |
| 3. Build Intelligent Multichannel Rails | Predictive routing sends each request through the optimal channel (API, portal, fax, or phone) with automated retries and error handling. | Fewer manual touches, fewer rejections, and accelerated submission throughput without workflow disruption. |
| 4. Create Predictive Dashboards | Live operational and financial dashboards quantify productivity, cost avoidance, revenue acceleration, and staffing efficiency. | Increases control over authorization bottlenecks, supports proactive staffing, and improves cash flow predictability. |
| 5. Continuously Refine Performance | Automated patient notifications and feedback loops retrain models as payer policies evolve. | Sustained denial reduction and first-pass approval improvement over time. |
The goal is straightforward: apply automation where the volume and financial impact are highest, and reserve human expertise for clinical judgment, peer-to-peer escalations, and exceptions.
Flow Auth was purpose-built for the real payer mix environments that dominate healthcare today, where fragmentation is the rule, not the exception.
The Business and Clinical ROI Other Health Systems Are Capturing
Health systems across the U.S using AI-powered multichannel automation like Flow Auth are already seeing measurable gains across cost, productivity, and patient outcomes.
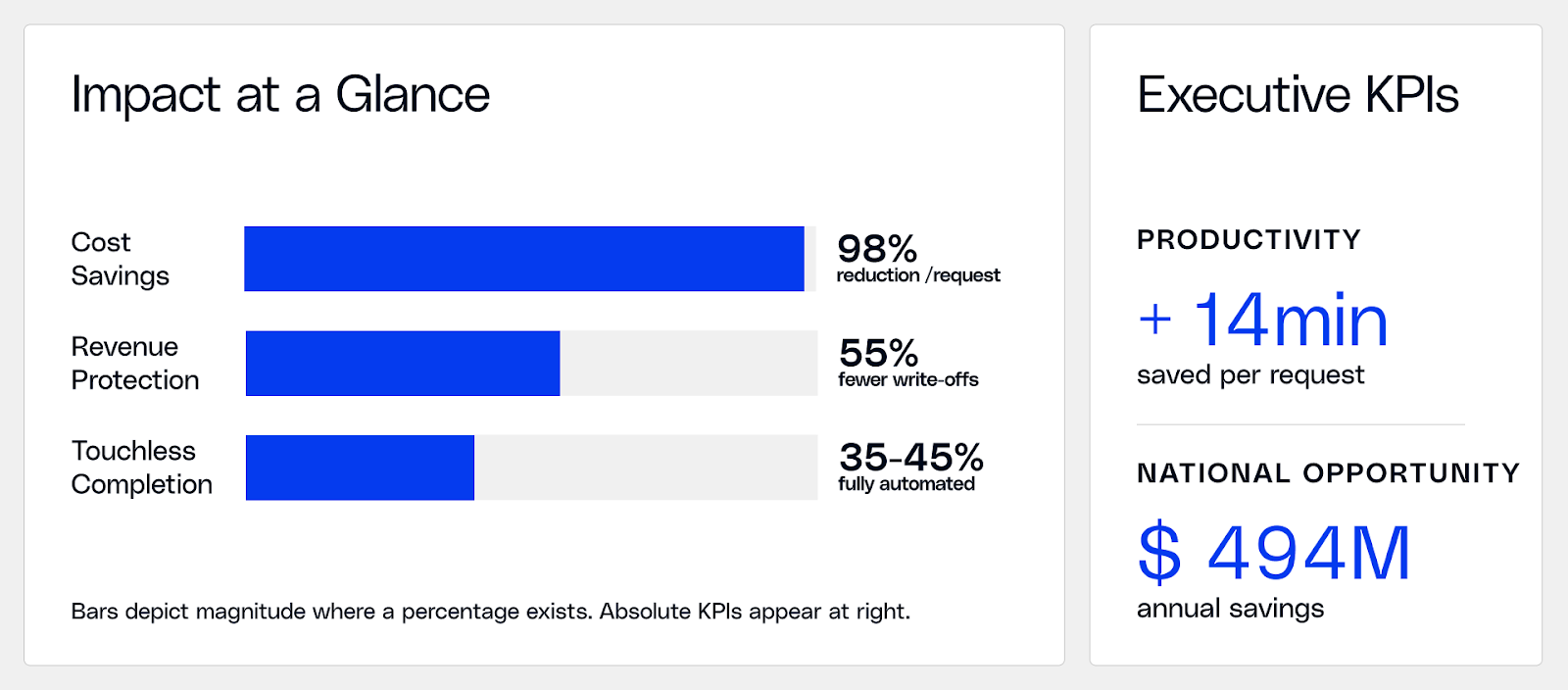
- 50-75% of manual tasks automated through AI-powered PA (McKinsey & Co.)
- 35% of prior authorizations fully automated with no human intervention (2024 CAQH Index Report)
- 14 minutes saved per request in staff time (2024 CAQH Index Report)
- $494M in annual savings across early adopters (2023 CAQH Index Report)
The Strategic Imperative
ePA is necessary, but not sufficient.
To manage the full payer mix, health systems need AI that adapts to each payer and keeps humans focused on care, not clerical work.
Flow Auth delivers exactly that:
An AI-driven, multichannel prior authorization platform that routes intelligently across APIs, portals, and legacy channels while predicting outcomes, reducing denials, and accelerating approvals.
Ready to See It with Your Payer Mix?
Flow Auth can analyze your actual authorization data to quantify immediate opportunities for cost reduction and revenue acceleration. Book a Demo

.png)





.png)









.svg)
.svg)

.svg)

