Prior Authorization Is A Strategic Asset

Prior authorization isn't broken. Our thinking about it is.
Every week, American medical practices complete 39 prior authorizations, burning 13 hours of staff time. That's nearly two full workdays lost to administrative friction. Meanwhile, 93% of physicians report that prior auth delays patient care, and 89% cite it as a major contributor to burnout.
These numbers tell a story of systemic failure. But they also reveal something else: we've been solving the wrong problem.
The Billion-Dollar Blind Spot
For years, healthcare organizations have approached prior authorization as a compliance burden to be minimized. The strategy has been simple: automate the paperwork, speed up the process, reduce the friction. Make the hamster wheel spin faster.
This approach fundamentally misunderstands what prior authorization represents.
Prior auth is the most granular, real-time interface between clinical decision-making and financial reality in healthcare. Every approval, denial, and delay generates strategic intelligence about payer behavior, documentation gaps, and revenue vulnerabilities. Yet most organizations treat this goldmine of data like waste to be processed as quickly as possible.
The real opportunity isn't to make prior auth hurt less. It's to make it work for you.
Reframing Prior Auth as Strategic Asset
When you stop seeing prior authorization as paperwork and start seeing it as intelligence, everything changes.
Those denial patterns reveal exactly where your clinical documentation falls short. Those approval delays show which payers are slow-walking your claims and costing you millions in delayed revenue. Those successful authorizations become your playbook for what works.
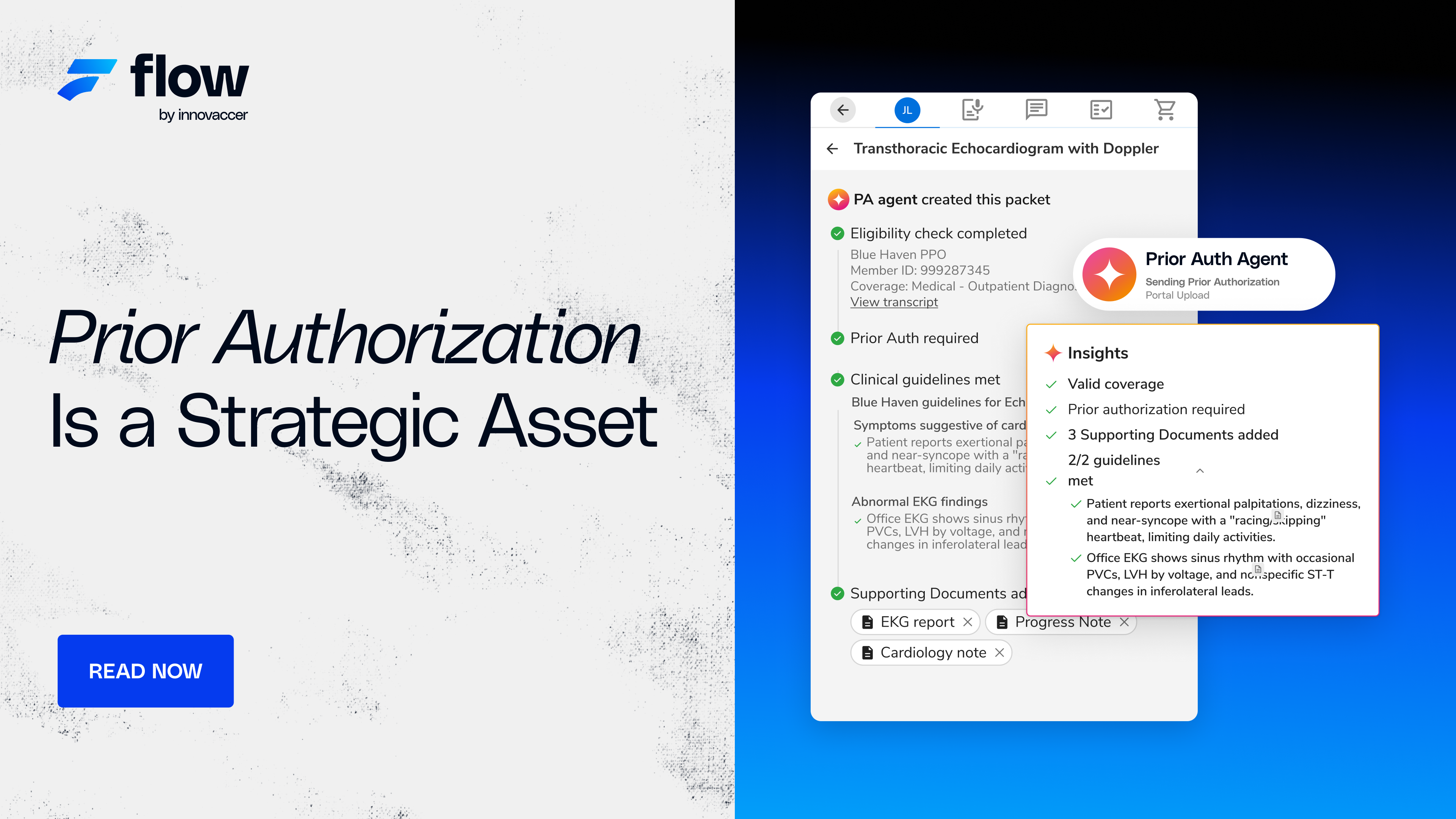
This is the premise behind Innovaccer's Flow Auth: prior authorization isn't just an administrative hurdle. It's a high-resolution lens into payer dynamics, patient access challenges, and revenue risks. More importantly, it's a growth engine hiding in plain sight.
The Three-Dimensional Value Creation
For Clinicians: Traditional prior auth forces physicians to guess what documentation might satisfy a faceless reviewer. Flow Auth provides real-time, payer-specific guidance at the point of care. Not generic best practices, but actual intelligence about what specific payers want to see for specific procedures. This isn't just automation; it's optimization. Requests become bulletproof before they're submitted, eliminating denial-and-resubmit cycles that drain clinical resources.
For CFOs: Prior authorization data is the earliest predictor of revenue risk in your entire operation. Days before a claim is submitted, prior auth already signals whether you'll get paid. Flow Auth transforms this data from operational noise into strategic signal. Suddenly, you can identify denial trends before they hit your revenue cycle, benchmark approval rates against peers, and use hard data in payer negotiations. When you can prove your approval rates are 15% below regional averages for identical procedures, you change the power dynamic with payers.
For Patients: Every prior auth delay represents continued pain, mounting anxiety, and potentially worsening conditions. Flow Auth's approach recognizes that operational excellence directly translates to patient trust. When you can guarantee authorization decisions quickly and communicate transparently, you're not just providing healthcare. You're building competitive advantage in a consumer-driven market.
The Compounding Value
Most healthcare IT solutions provide linear returns: invest X, receive Y. Flow Auth creates something different: a value flywheel that accelerates over time.
Automation eliminates grunt work, freeing staff to focus on complex cases that need human intelligence. As the system learns from every authorization, documentation quality improves systematically across the organization. Better documentation drives faster approvals, which means patients get care sooner and schedules run smoother. All of this generates rich data that feeds back into the system, revealing patterns humans would never catch and opportunities that were previously invisible.
The flywheel spins faster with each rotation. Prior auth transforms from your biggest operational headache into a strategic advantage competitors can't match.
The Leadership Playbook for 2025
Healthcare organizations that will thrive won't be those that digitize fax machines faster. They'll be those that fundamentally reimagine what prior authorization can be.
Elevate Metrics to the Boardroom: Denial rates, approval speeds, and first-pass success rates belong on executive dashboards alongside patient satisfaction and operating margins. They're leading indicators of both. When prior auth metrics slip, revenue and patient experience are about to crater.
Create Cross-Functional Ownership: Prior authorization touches clinical care, revenue cycle, patient experience, and payer relations. Stop letting it fall through organizational cracks. Build cross-functional teams with shared accountability. When clinicians, revenue leaders, and patient experience executives own the same outcomes, transformation happens.
Convert Data into Leverage: Every denial is intelligence. Aggregate enough intelligence, and you have power. Track your prior auth data, benchmark it, analyze it, then weaponize it. Walking into payer negotiations with evidence of systematic approval disparities changes the conversation from supplication to confrontation.
Make Excellence Your Brand: In a world where patients can switch health systems with a click, operational excellence becomes brand differentiation. The health system that guarantees 24-hour prior auth decisions doesn't just reduce administrative burden. It becomes the destination of choice.
The Strategic Imperative
Prior authorization isn't going away. As healthcare costs climb and expensive therapies proliferate, it will likely intensify. We can rage against this reality, or we can transform it into opportunity.
Flow Auth represents this transformation. Within the administrative burden of prior authorization lies unprecedented strategic potential: granular understanding of payer behavior, systematic improvement of clinical documentation, prediction and prevention of revenue cycle problems, and delivery of seamless patient experiences that build lasting loyalty.
The organizations that grasp this opportunity won't just survive prior authorization. They'll use it as a springboard to build more intelligent, responsive, patient-centered health systems. They'll turn their biggest operational challenge into their strongest competitive advantage.
The revolution in prior authorization has arrived. The question isn't whether you can afford to rethink prior authorization. It's whether you can afford not to. While you're treating it as paperwork, your smartest competitors are turning it into a growth engine.
And in healthcare's rapidly evolving landscape, that's the difference between leading and being left behind.
Get a closer look at Flow Auth at go-flow.ai

.png)





.png)









.svg)
.svg)

.svg)

