Top Capabilities of an AI-Powered RCM Solution in 2026


Revenue Cycle Management is not just about getting claims out the door anymore. In 2026, healthcare organizations are expected to move faster while meeting stricter payer expectations, growing administrative load, and rising pressure to standardize data exchange and prior authorization workflows.
That is why the conversation has shifted from basic automation to operational autonomy. The best Revenue Cycle Management Software is no longer measured only by how many tasks it automates. It is measured by whether it can understand clinical context, interpret payer requirements, execute workflows consistently, and improve outcomes over time.
This blog breaks down the top capabilities that define an AI-powered RCM solution in 2026, and how to evaluate Revenue Cycle Management Companies and platforms using a practical lens.
What is revenue cycle management?
If you still get the question “What is revenue cycle management,” here is the simplest definition.
Revenue Cycle Management is the end-to-end set of processes healthcare organizations use to capture, manage, and collect patient service revenue. It starts with eligibility and authorizations, then moves through billing and coding, claims submission, denial management, payment posting, reconciliation, and collections.
In 2026, the scope stays the same. The performance standard changes. Healthcare revenue cycle management is increasingly judged by how well teams prevent avoidable rework, reduce denials, and accelerate cash, without increasing burnout.
Why AI-powered RCM matters more in 2026
RCM teams are dealing with three realities at the same time.
First, payer requirements continue to evolve and vary widely. Second, the volume and complexity of prior authorizations remains a major operational bottleneck. Third, the industry is moving toward higher expectations for electronic data exchange between providers and payers.
Put together, that means RCM leaders cannot afford workflows that rely on tribal knowledge, manual follow-ups, and rework-heavy exception handling. AI becomes valuable when it turns those workflows into repeatable, trackable, and continuously improving execution.
Top capabilities of an AI-powered RCM solution in 2026
Instead of a long feature list, it helps to think in four layers. Strong platforms build all four. Weak platforms over-invest in one and ignore the rest.
Layer 1: The foundation that makes automation reliable
Unified data plus workflow orchestration
AI cannot improve Revenue Cycle Management if it cannot see complete context. A modern platform must unify clinical signals, payer rules, authorization status, claim history, and operational workflows so the system can make the right decision at the right time.
This capability matters because disconnected point solutions create brittle automation. When payer policies shift or documentation standards change, rules break and the team ends up doing more manual work than before.
Layer 2: Front-end precision that prevents revenue leakage
Eligibility verification that runs early
A 2026-ready platform should verify coverage and eligibility early enough to prevent downstream disruptions. When eligibility issues are caught late, the result is avoidable denials, patient confusion, delayed care, and slow cash.
This capability is foundational for Revenue Cycle Management Healthcare because many denial patterns are created upstream long before a claim is submitted.
Prior authorization automation that is payer-smart
Prior auth is where AI either delivers real ROI or becomes another tool that creates additional steps. The best solutions do not rely only on templates or static rules. They adapt to payer requirements and use clinical evidence intelligently.
A strong AI-powered RCM solution should be able to:
- Detect prior auth needs early by monitoring orders and schedules and checking payer guidelines
- Assemble payer-ready packets from EHR evidence such as notes, labs, and imaging
- Submit through available electronic and non-electronic routes, then track status changes continuously
- Generate appeal packets when required and route them to the right team or workflow
This is critical for Hospital revenue cycle management because authorization delays and denials slow care and delay reimbursement.
Layer 3: Middle-cycle intelligence that improves claim quality
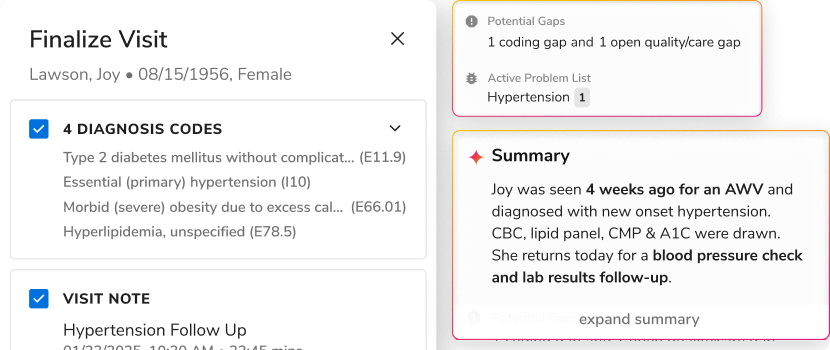
Medical necessity intelligence as a continuous state
In 2026, medical necessity cannot be treated as a one-time checkbox. The strongest solutions treat it as a continuously validated state that updates as documentation, clinical signals, and payer criteria evolve.
This is the difference between automation that submits more and automation that gets approved more.
Billing and coding that is clinically aligned
Billing and coding remains a major lever, but it has to work like clinical intelligence, not just coding throughput. Platforms should connect coding quality to documentation quality and payer expectations so that issues are identified before submission.
This capability directly impacts revenue cycle management in medical billing because missed specificity often turns into denials, underpayments, or manual rework.
Claims management designed for clean submission
Claims management in 2026 is not just creating claims. It is cleaning, validating, and submitting claims with fewer errors and fewer avoidable exceptions, then learning from payer outcomes.
Strong Revenue Cycle Management Software should include pre-submit validations that reflect payer logic and historical denial drivers, not only generic checks.
Layer 4: Back-end execution that speeds up cash and reduces rework
Denial prevention plus appeals automation
Denials should be treated like a product problem. Patterns should be detected early, categorized accurately, routed correctly, and resolved with minimal manual effort.
A modern platform should support denial prevention and denial operations, including generating appeal narratives and assembling supporting documentation.
This is one of the biggest areas where Revenue Cycle Management Companies often lean on services-heavy approaches. In 2026, buyers increasingly prefer platforms that reduce dependence on manual denial work.
Payment posting and reconciliation that closes the loop
A modern platform should automate payment posting where possible and reconcile what was paid versus what should have been paid at scale.
This capability is essential for scaled Healthcare revenue cycle management because reconciliation is where hidden leakage accumulates and where operational teams lose time.
Revenue intelligence that drives action
Dashboards are not enough. The best platforms surface real-time insights tied to operational action, such as where cash is stuck, which payer policies have shifted, which specialties are generating rework, and what to fix first.
In 2026, the value of revenue intelligence is directly tied to whether it changes workflow behavior, not whether it produces more reports.
How to evaluate Revenue Cycle Management Software in 2026
If you are comparing Revenue Cycle Management Companies or platforms this year, these questions will separate AI-washed automation from real performance improvements:
- Does the platform unify clinical, payer, and operational context, or does it depend on disconnected tools?
- Can it improve first-pass outcomes in prior auth and claims, or does it simply move work around faster?
- Does it adapt to payer requirement changes without constant manual reconfiguration?
- Does it reduce denial volume through prevention, not just improve denial handling speed?
- Does it close the loop through payment reconciliation and outcome learning, or does learning stay trapped in spreadsheets and people’s heads?
In 2026, the strongest Revenue Cycle Management programs will not be defined by how many people they can throw at work queues. They will be defined by how consistently their systems prevent rework, validate medical necessity, and execute payer workflows with minimal manual follow-up. That is the real promise of an AI-powered RCM solution: not replacing teams, but giving teams an operational layer that keeps learning, keeps adapting to payer variability, and keeps cash moving.
As Hospital revenue cycle management evolves under growing authorization and interoperability pressure, the platforms that win will be the ones that bring together clean data, intelligent workflows, and measurable outcomes across billing and coding, claims management, denials, and reconciliation.
Read more about The Real Reasons Revenue Cycle Investments Aren't Paying Off: https://go-flow.ai/resources/blogs/the-real-reason-your-revenue-cycle-investments-arent-paying-off

.png)



.png)









.svg)
.svg)

.svg)

