Fix the Note, Fix the System: Reduce Burnout, Bottlenecks, and Hidden Losses

Walk into any healthcare organization today and you can feel the strain before anyone says a word. Providers move through their day carrying the weight of documentation: clicking, copying, reconciling, and re-creating information that already exists somewhere in the system.
For every 8 hours of scheduled patient care time, ambulatory physicians spend approximately 5.8 hours actively working in the EHR, with documentation consuming 2.3 hours per 8 patient care scheduled hours.
If you sit in an operational or clinical leadership role, you feel the consequences ripple through your entire ecosystem: billing cycles slow, CDI teams work backward instead of forward, quality teams chase data that should already be structured.
What begins as a documentation challenge becomes an operational bottleneck.
Starting in 2026, CMS fully transitions to the V28 HCC model, removing over 2,200 diagnosis codes and expanding HCC categories from 86 to 115. V28 demands clinical specificity details like ejection fraction percentages and NYHA classification must be documented during the patient encounter, not added after the fact. This shift increases compliance and revenue risks for organizations relying mainly on post-encounter CDI workflows.
When documentation quality improves at the point of care, organizations see measurable improvements across throughput, burnout, revenue integrity, and quality metrics. Not through workflow redesign, but through fixing the upstream information architecture that downstream processes depend on.
Where Does Clinical Documentation Actually Break Down?
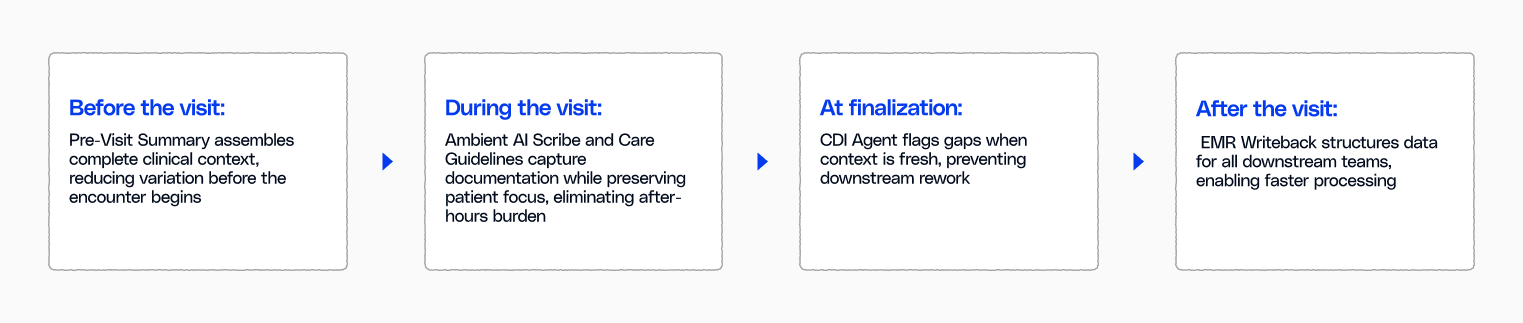
Trace any operational bottleneck back to its source, and you'll find the pattern: information enters the system inconsistently, incompletely, or unstructured. The breakdown happens at four precise moments in the clinical workflow, and each creates friction that multiplies downstream.
Before the visit: When fragmented prep determines the day's outcome
Your physician logs in early and opens the first chart. Eight months of documentation sprawl across the screen: a cardiology consult buried in narrative, medication changes requiring reconciliation, care gaps invisible without manual searching. Fifteen minutes to synthesize it all before the patient walks in.
This is where variation begins, not from lack of clinical skill but from fragmented information architecture. Care gaps get identified or missed based on which tabs get opened, whether scanned PDFs get reviewed, and how much context can be reconstructed before time runs out. The visit outcome depends entirely on information access, not clinical competence.
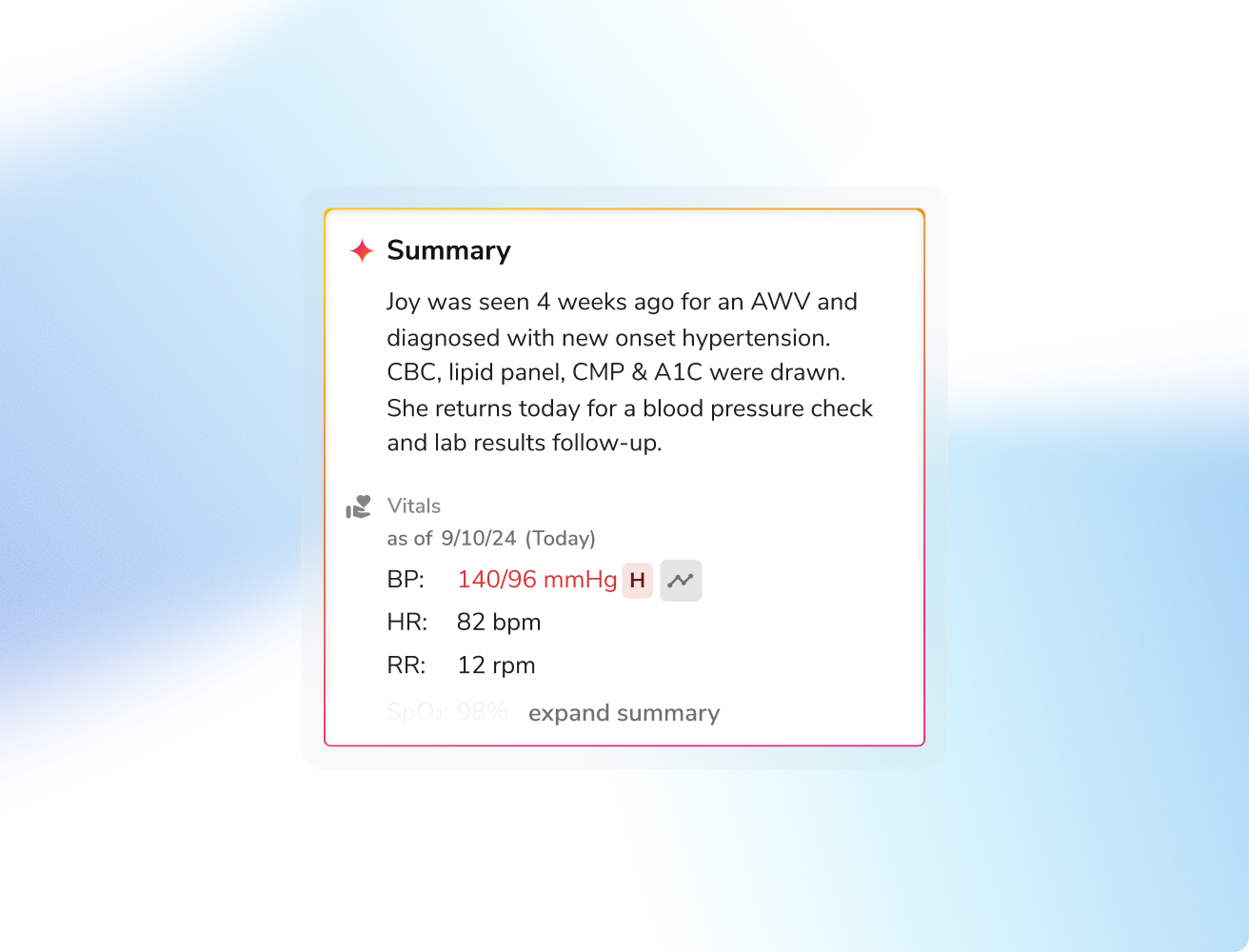
The Pre-visit Summary surfaces relevant patient history, labs, medications, and clinical conditions from all data sources, including the unstructured data that typically stays buried. When your physician opens the chart at 6:45 AM, the clinical picture is already assembled with medication adherence trends, specialist summaries extracted, open care gaps flagged, and risk stratification calculated. The preparation that used to take fifteen minutes is already complete.
During the visit: when cognitive load decides what gets captured
Three patients into the morning, cognitive load peaks. The provider must simultaneously listen, examine, diagnose, and document in real time. Under this pressure, specificity suffers.
A patient with heart failure gets documented as "heart failure" instead of "heart failure with reduced ejection fraction, NYHA Class III." The difference matters for risk adjustment, but in the moment, clinical reasoning takes precedence over coding language.
Meanwhile, care guidelines remain buried in separate tools, so the colorectal cancer screening the patient qualifies for, never surfaces during an encounter already focused on acute symptoms.
This is where documentation quality diverges, from competing cognitive demands. Research using EHR audit logs confirms that documentation and clerical tasks consume 44% of total EHR time, creating cognitive overload that impairs both documentation specificity and clinical decision-making.
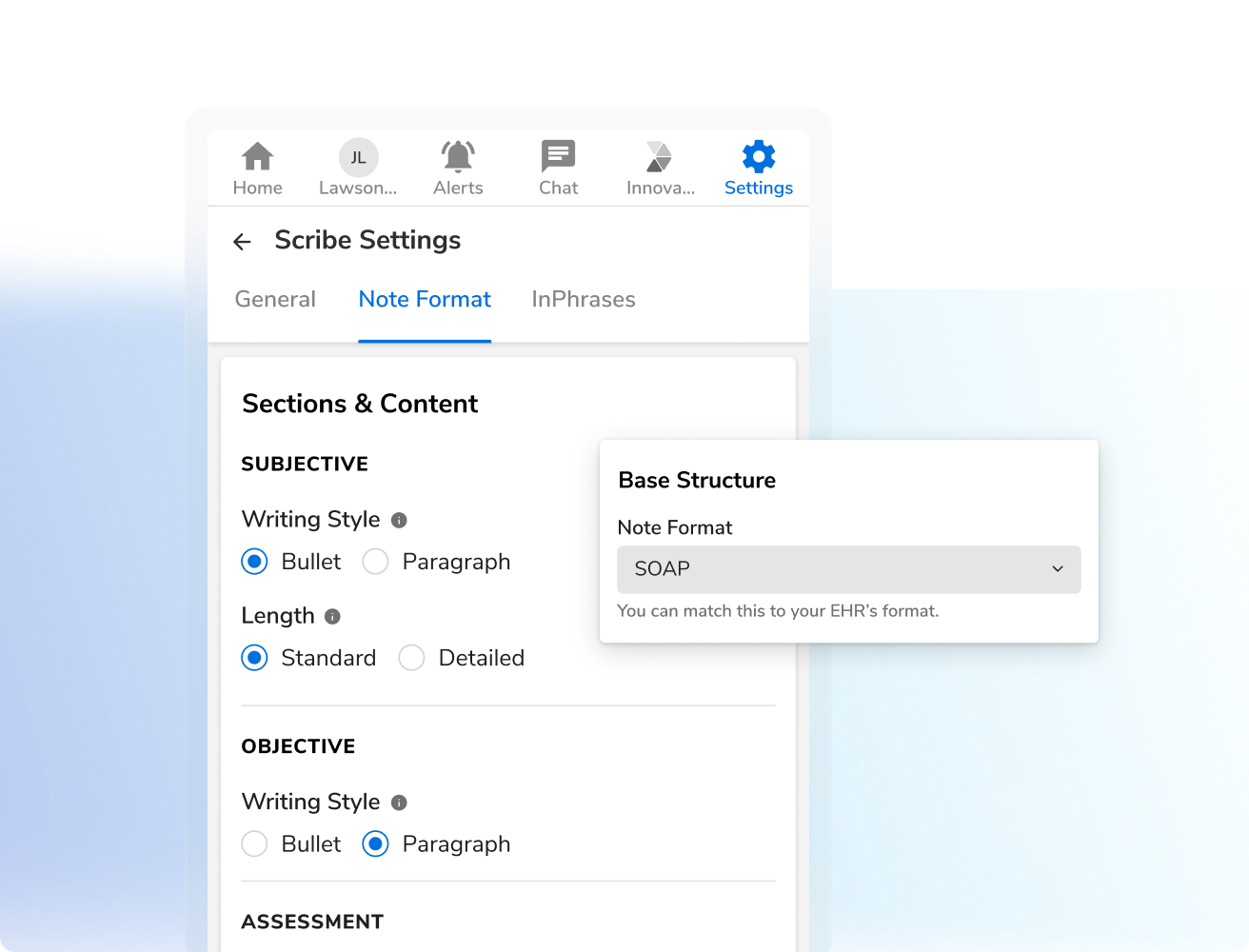
Ambient Scribe captures the conversation in real time and generates a structured SOAP note, allowing the physician to focus on clinical reasoning rather than documentation mechanics. Specialty-specific templates adapt automatically so the cardiologist sees NYHA classification prompts while the primary care physician gets HbA1c trends and ICD-10 specificity guidance, all without interrupting the patient conversation.
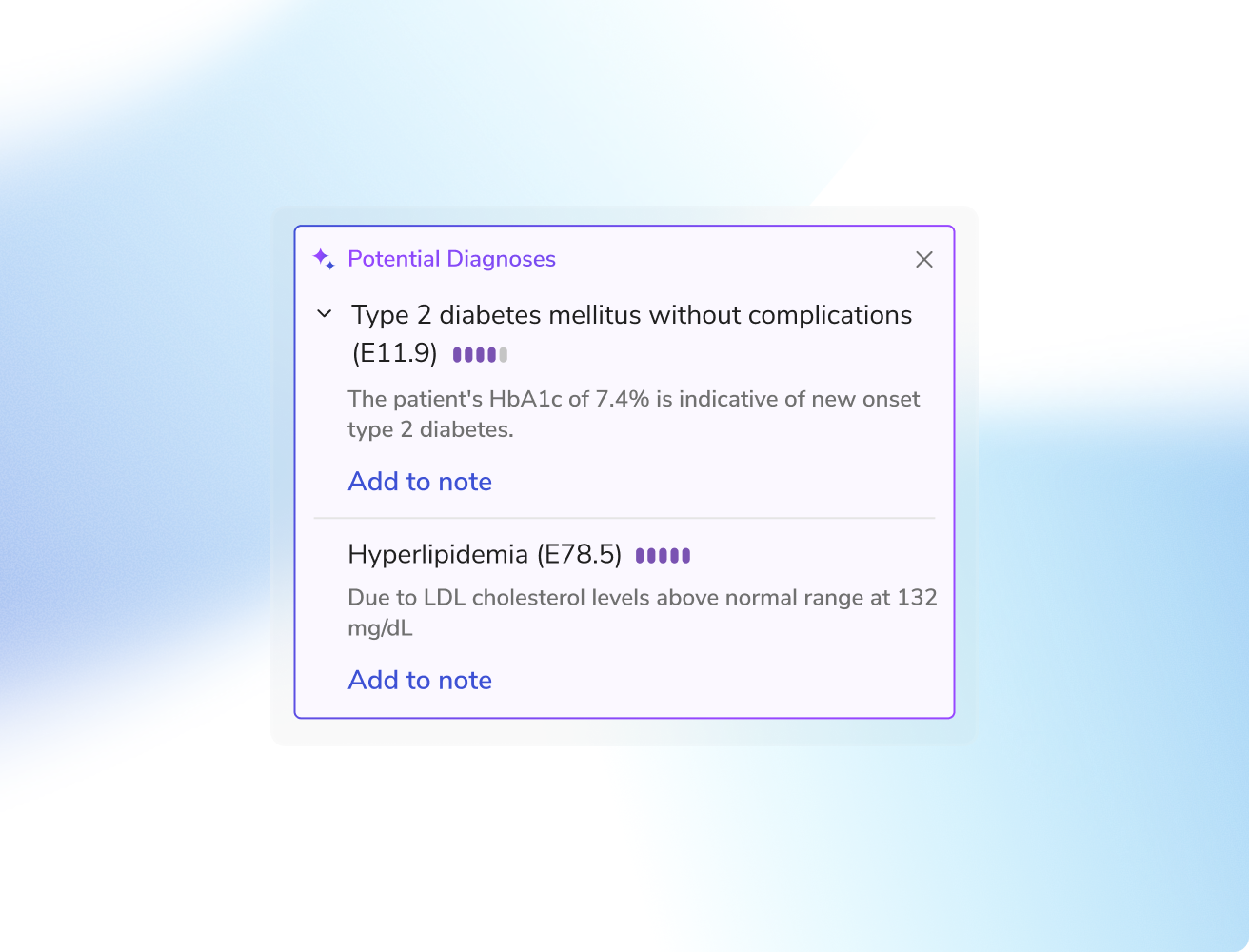
Care Guidelines surface evidence-based recommendations at the exact moment they inform decisions, ensuring care gaps get addressed when the patient is present rather than flagged in retrospective review weeks later. The cognitive load that used to force trade-offs between patient engagement and documentation accuracy disappears.
After the visit: when delayed documentation becomes permanent gaps
The waiting room is empty, but your provider remains at the desk. In 2024, 22.5% of physicians reported spending more than 8 hours per week on the EHR outside normal work hours, i.e. uncompensated time that extends far beyond any individual encounter.
Encounters that felt clear at 10 AM have faded by evening. The clinical nuances that informed treatment decisions during the visit now exist only in memory, while the documentation system demands precise severity descriptors and coding language that wasn't prioritized during patient care.
This is where documentation gaps become permanent, not from lack of clinical thoroughness but from the inherent limitations of memory-based documentation. The specificity that matters for risk adjustment exists in the physician's mind during the encounter but deteriorates over hours through no fault of their own.
By the time your CDI team identifies missing MEAT elements days later, the clinical context has evaporated entirely. What could have been resolved in seconds during finalization becomes lengthy query cycles that consume both CDI capacity and physician goodwill. This is where concurrent CDI intervention changes the dynamic.
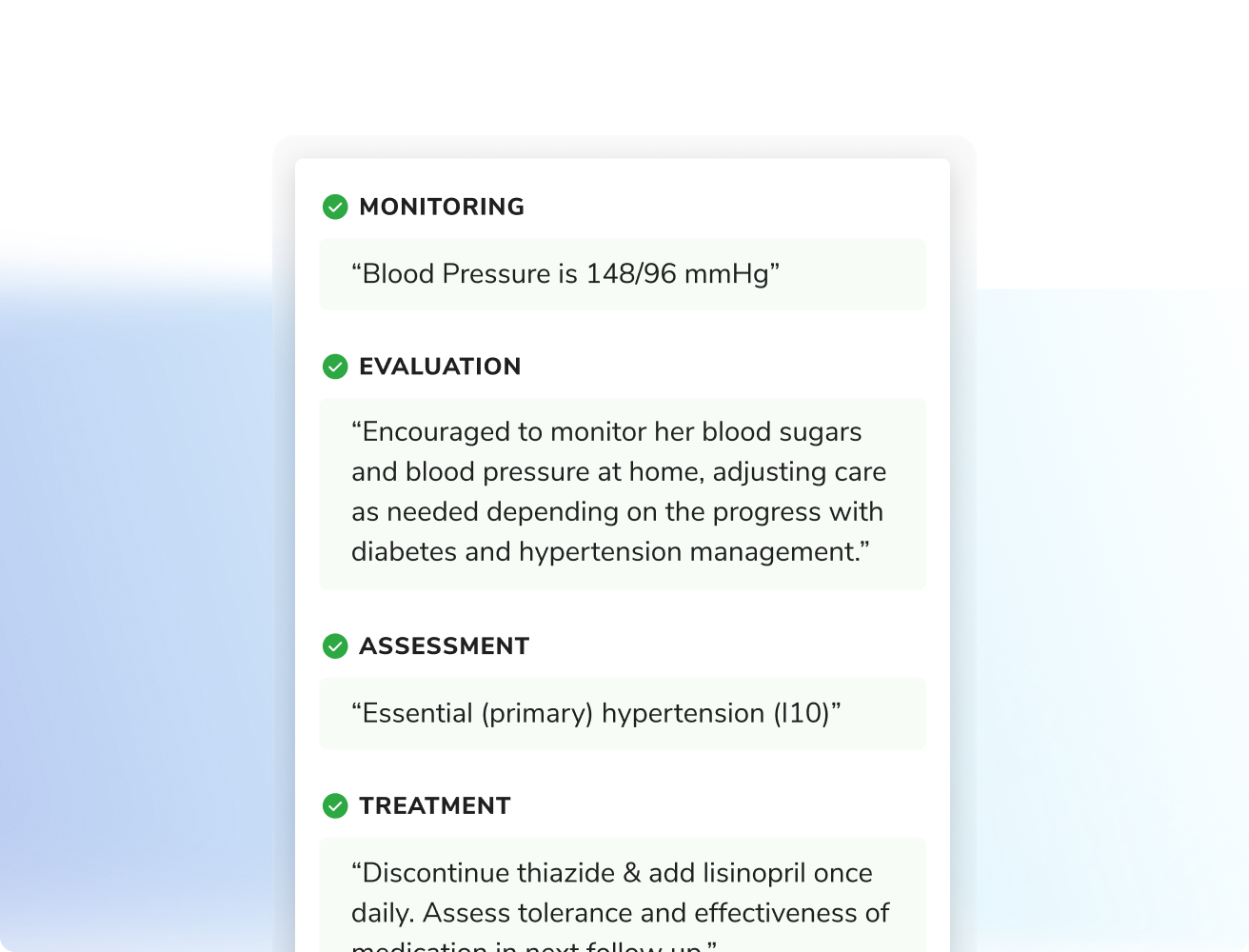
CDI Agent identifies documentation gaps while clinical context is fresh, enabling concurrent review. This shifts CDI focus from reactive query cycles to concurrent optimization, reducing query volume and accelerating first-submission acceptance rates.
Research shows primary care physicians spend a median of 6.2 minutes per visit on after-hours EHR work; what researchers term 'pajama time.' On unscheduled days, some physicians log over 2.8 hours completing documentation that couldn't be finished during clinic hours.
Days later: when unstructured notes force manual rework
When documentation gaps reach CDI teams days or weeks after discharge, specialists must initiate formal query processes: structured requests for clarification that require clinical indicators from the health record and provider response documentation.
These retrospective query cycles consume CDI capacity, delay billing submission, and require physician time to reconstruct clinical context that has already faded.
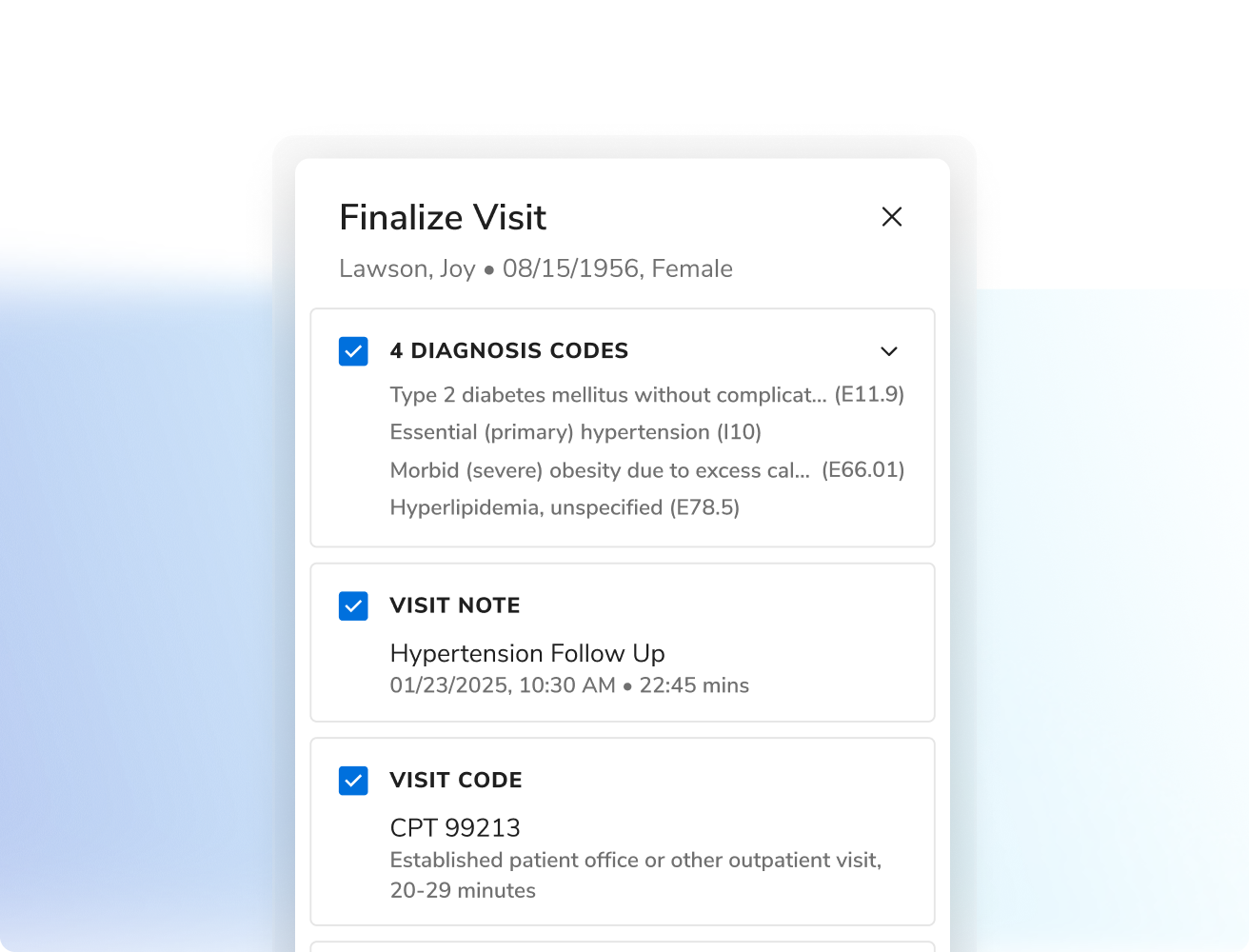
EMR Writeback structures the information at the point of capture so it flows directly into the fields your downstream teams need. Problem lists populate with appropriate specificity, quality measures trigger without abstraction, and care management workflows begin with structured tags already in place.
The same visit that used to require manual processing by three different teams now feeds each downstream function automatically, allowing experienced staff to focus on complex cases rather than data extraction.
How Provider Copilot Improves Documentation at Every Stage and Transforms Your Clinical Workflow
National longitudinal research tracking 18,265 ambulatory physicians found that high-intensity adoption of team-based documentation support reduced physician documentation time by 28.1% while increasing visit volume by 10.8%. Provider Copilot achieves this through four concurrent interventions at the critical moments where documentation quality determines downstream outcomes.
Address these four breakpoints at their source, and the benefits multiply across every downstream function without requiring your teams to change how they work.
The result is operational velocity that wasn't possible when documentation remained fragmented and unstructured.
Billing cycles tighten as claims move directly to submission. CDI workload shifts from firefighting to optimization. Physicians finish their workday when the last patient leaves, not three hours later.
This isn't a redesign requiring months of change management. It's a targeted intervention at the four moments where documentation quality determines everything downstream.
Flow's Provider Copilot integrates with 80+ EMRs through both native API connections and standard HL7 interfaces, with custom configuration required to map specialty-specific documentation fields to downstream quality and revenue cycle systems.
Calculate Your ROI: See What Provider Copilot Means for Your Operation
Flow's Provider Copilot addresses all four breakpoints without requiring teams to change how they work.
Use the ROI calculator to answer a few questions about your office type, provider count, and specialty mix. See your projected savings including estimated ROI, revenue from accurate CDI, and cost savings from reduced turnover and administrative burden.
Or request a demo to see how Provider Copilot strengthens your documentation infrastructure in action.

.png)





.png)









.svg)
.svg)

.svg)

