The $500B AI Opportunity: How Healthcare CFOs Can Transform Administrative Burden into Competitive Advantage


Healthcare’s financial leaders are staring down at a paradox. On one hand, the US health system wastes $528 billion annually, almost 1.8% of the GDP, on administrative work that doesn’t add any real value to patient care. On the other hand, advances in artificial intelligence (AI) now give CFOs an unprecedented opportunity to convert this burden into a source of long-term financial advantage.
For CFOs, the stakes are high. Administrative waste is a nuisance, but it's also a direct burden on margins, growth, and enterprise value. Leaders are now viewing administrative processes through the lens of AI. They are treating waste reduction as a strategic lever, automating inefficiencies at scale and redirecting resources towards innovation.
Why Administrative Burden is a Strategic CFO Problem
Consider what happens today with every $100 that passes through the system. By the time it passes through insurers and providers, only $68 actually reaches the front lines of patient care. The rest is diverted into layers of paperwork and redundant approvals, primarily because of a redundant system.
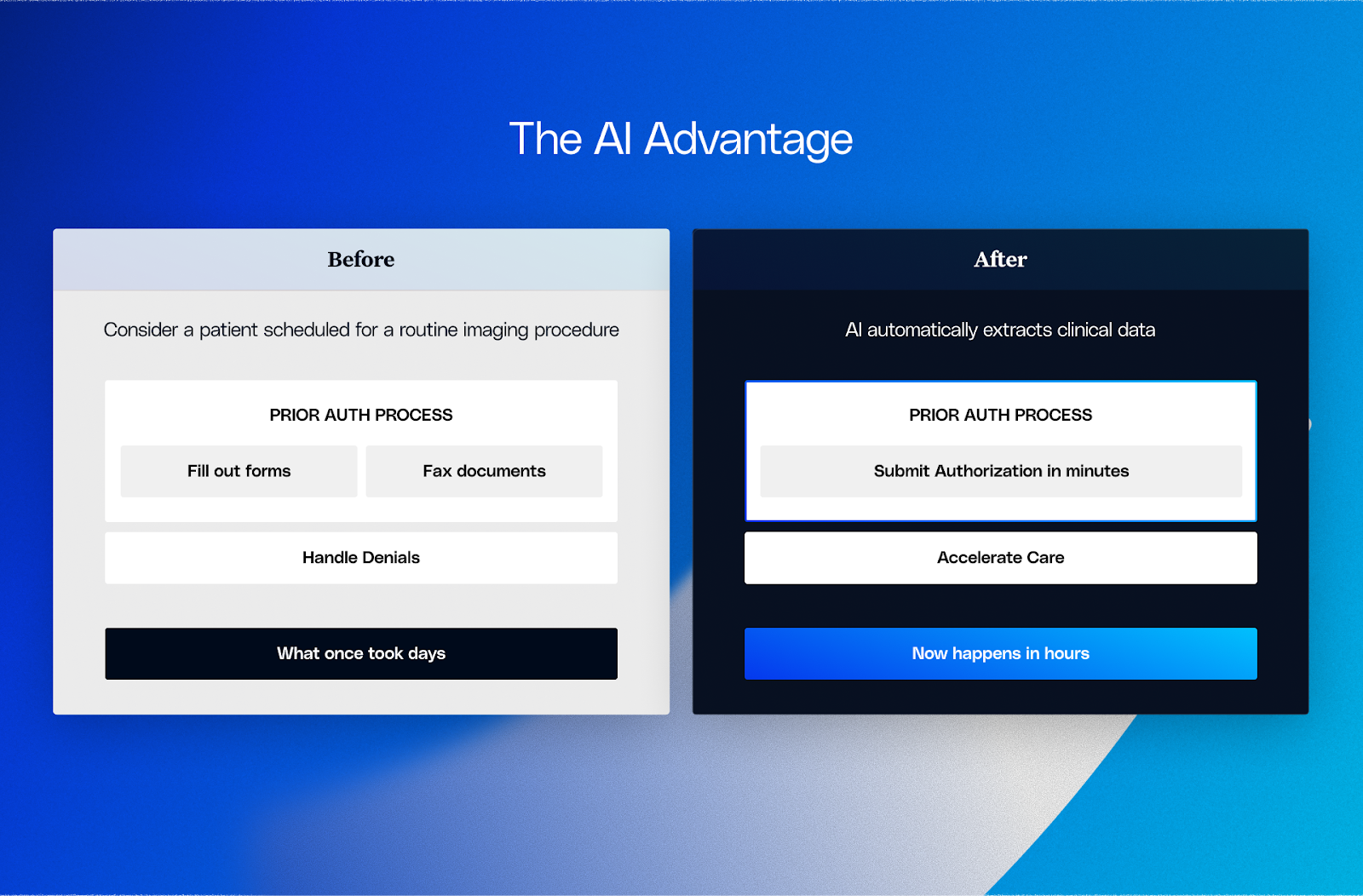
Imagine a patient coming in for a routine procedure. Their clinician spends more time navigating fragmented prior authorization workflows than speaking with them. The claim then bounces between insurer portals, faxes, and call centers before finally landing in a hospital billing department that devotes nearly one in every five dollars it receives to administration. By the time the patient’s care is paid for, nearly a third of the money that should have supported their health has been consumed by inefficiency. In most cases, these manual prior auth processes delay care and drain staff productivity.
CFOs know these aren’t abstract costs. They hit the bottom line with thinner margins and heavier pressure on staff. They also block capital from being used where it matters most, whether that’s new technology, service expansion, or stronger patient care.
From Cost to Advantage: The AI Opportunity
What makes 2025 different is the maturity of enterprise-grade AI automation. Unlike traditional RPA or isolated point solutions, AI platforms can handle complex judgment-driven processes at scale. This turns administrative overhead from a burden into a strategic advantage.
AI can:
- Analyze large amounts of unstructured data: It is able to read and extract information from a variety of sources, including faxes, PDFs, scanned documents, EHR notes, and lab reports. This tremendously saves staff hours on manual data entry and reduces the risk of human error when first-time claims and authorizations are processed.
- Automate judgment-heavy tasks: Beyond simple rule-based work, AI can assess medical necessity, validate documentation, and complete automated prior authorization submissions or denial resolutions that previously required human review. This frees up clinical and revenue-cycle staff for higher-value work. This is where AI prior authorization software and touchless prior authorization capabilities are redefining what efficiency looks like in the revenue cycle.
- Constant learning from interactions: AI gets smarter with each payer-provider interaction, developing accuracy and recognizing denial patterns while forecasting payer responses. It establishes a self-correcting process that reduces mistakes and speeds approvals.
- Provide actionable insights for financial decisions: With real-time visibility, CFOs can see where claims bottlenecks exist and where workflow is inefficient, which allows them to intervene proactively, rather than reactively.
A Strategic Roadmap for CFOs
Turning administrative ineffectiveness into a measurable value starts with a strong CFO-led process. Here's how:
- Baselining the Burden
Consider administrative inefficacy as an item on the P&L, and quantify the actual expense across denial, claims, prior authorizations, and the workforce. - Prioritize High-Impact Areas
Start with functions where AI yields immediate ROI, such as claims processing, eligibility checks, and electronic prior auth. The right prior authorization platform can automate the full cycle from request to payer response, drastically reducing turnaround time.
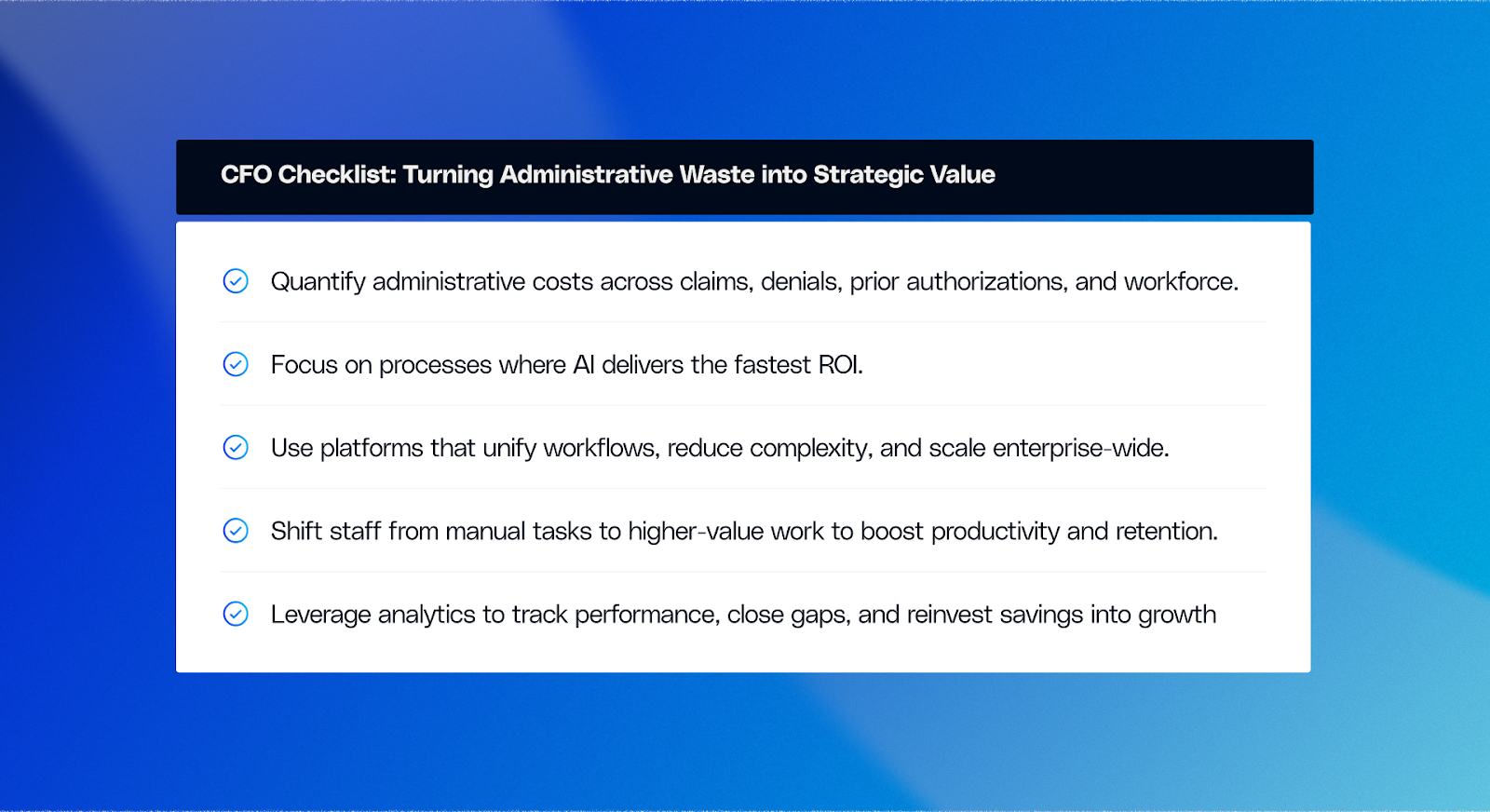
- Deploy AI Platforms, Not Point Solutions
Layering tools creates complexity. Instead, invest in platforms that unify automation across workflows, integrate with existing systems, and scale enterprise-wide. - Redesign Workforce Strategy
Redeploy FTEs from manual work to higher-value activities. This not only boosts retention but also enhances productivity. - Build a Continuous Improvement Loop
Use AI-driven analytics to track performance, close gaps, and reinvest the savings into innovation and growth.
Also read: Healthcare organisations are losing millions to Prior Authorization inefficiencies and here's how to stop it.
Seizing the $500B Opportunity
For healthcare CFOs, the completion of eliminating the $500B administrative waste challenge is not just an unavoidable cost of operations. It represents an extraordinary opportunity. The maturity of AI platforms in 2025 will enable leaders to move beyond temporary solutions and achieve enduring competitive advantage.
By thinking of administrative work as a strategic lever, or tool, CFOs will be able to recoup lost revenues, ease workforce pressures, and invest money and time into growth and patient care. Those who are ambitious enough to move forward now will not only reduce costs but will also evolve the financial and operational underpinnings of healthcare for the next decade.

.png)





.png)









.svg)
.svg)

.svg)

